|
Brain HypertensionBrain hypertension can cause severe brain disorders and anomalies. It is vital to be aware of this. Please read this research article written by Dr. Ruby Chang and Dr. Stephen Chan on WebMD in their E-medicine newsletter. This is a professional research paper but you will get the point. It is vital to maintain a blood pressure at or slightly below the recommended normal level of 120/80. Brain, Hypertensive Hemorrhage Author: Ruby Chang, MD, Staff Physician, Department of Radiology, New York Presbyterian HospitalCoauthor(s): Stephen Chan, MD, MBA, MPH, Consulting Staff, New York State Psychiatric InstituteContributor Information and Disclosures Updated: Apr 14, 2009 Overview Spontaneous intracranial hemorrhage affects approximately 40,000 people in the United States each year, comprising 10-20% of stroke occurrences. In adults who present with nontraumatic intraparenchymal hemorrhage in the brain, hypertension is the most common etiology. Intracerebral hemorrhage (ICH) occurs when damaged arteries bleed directly into the brain substance.
For excellent patient education resources, visit eMedicine's Stroke Center. Also, see eMedicine's patient education article Stroke. Pathophysiology Increased blood pressure damages the cerebral vessels primarily in 2 ways:
•Plasma leakage from persistently elevated blood pressures also can result in hyaline degeneration of the cerebral blood vessels. Serum protein accumulates in the basement membranes of the arterioles and results in collagen formation. Arterial sclerosis and fibrinoid necrosis may occur, as well as focal aneurysmal dilatation (Charcot-Bouchard intracerebral microaneurysm). Two theories about the mechanism of intracranial bleeding related to hypertensive small-vessel disease have been developed as follows:
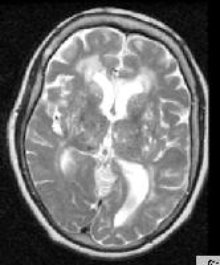
•The second theory states that brain infarction eventually results in vascular compromise. The first theory, intraparenchymal hemorrhage secondary to rupture of the vessel, is accepted more widely. Frequency United States Spontaneous intracerebral hemorrhage causes 10-20% of strokes and 15-20% of stroke-related deaths. The overall incidence of ICH is estimated to be 9 per 100,000. Of these patients, 70-90% have high blood pressure. International Approximately 10-18% of deaths in Western Europe result from intracerebral hematomas.4 The incidence and death rate in Japan is 4-6 times higher than in Western Europe and the United States. The higher rate in Japan may be related to diet, as a decrease in overall incidence of intracerebral hemorrhage has been associated with westernization of the Japanese diet after World War II. In a prospective, population-based Italian study by Sacco et al, 549 patients with intracerebral hemorrhage were studied to determine incidence, prognosis, and case fatality. The case-fatality rates were 34.6% at 7 days; 50.3% at 30 days; and 59.0% at 1 year. Increased risk for 7-day and 30-day mortality was associated with the presence of diabetes mellitus and posterior fossa hemorrhage; increased 30-day mortality was associated with older age of patients.5 A New Zealand population-based study by Feigin et al evaluated worldwide incidence and case fatalities of stroke from 1970 through 2008 and found that countries with low to middle incomes (based on World Bank classifications) had a 20% greater incidence of stroke than high-income countries. Over the previous 40 years, high-income countries had a 42% decrease in the incidence of stroke, whereas low- to middle-income countries had a greater than 100% increase in stroke incidence.6 Mortality/Morbidity According to reports, stroke is the third most common cause of mortality in the United States and may be responsible for approximately 2-4% of deaths. Spontaneous intracerebral hemorrhage causes 10-20% of strokes and 15-20% of stroke-related deaths. In a prospective, population-based Italian study by Sacco et al, 549 patients with intracerebral hemorrhage were studied to determine incidence, prognosis, and case fatality. The case-fatality rates were 34.6% at 7 days; 50.3% at 30 days; and 59.0% at 1 year. Increased risk for 7-day and 30-day mortality was associated with the presence of diabetes mellitus and posterior fossa hemorrhage; increased 30-day mortality was associated with older age of patients.5 Race The incidence of spontaneous ICH may be higher among black persons than white persons, since a higher incidence of hypertension is seen in black persons younger than 45 years. Sex Men have a 5-20% higher incidence of ICH than women. Age Of spontaneous intracerebral hemorrhage patients, 90% are older than 45 years. Anatomy The arteries in the brain damaged by exposure to chronic hypertension typically are the perforator arteries, which serve the basal ganglia, thalamus, and pons. Other areas that also may be affected include the centrum semiovale and, occasionally, the cerebellum. The areas with arteriolar damage are prone to lacunar infarcts and hypertensive hemorrhages. The areas in which hypertensive hemorrhages most commonly occur are the basal ganglia and thalamus (see Image 1). Predominantly, hemorrhages of the basal ganglia involve the putamen and are fed by the lenticulostriate arteries. Complications of focal hemorrhages include edema, ischemia, and infarct. If the hemorrhage is large enough and in the appropriate location, it may result in noncommunicating or obstructive hydrocephalus by compressing the foramen of Monro, the third ventricle, or the aqueduct of Sylvius. In contrast, extension of a parenchymal bleed into the ventricles may result in communicating hydrocephalus.
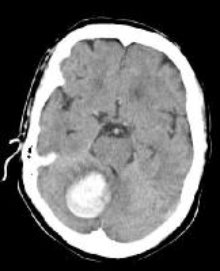
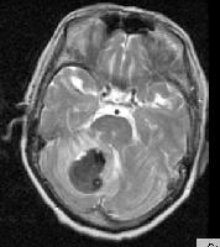
Secondary intraventricular hemorrhage (IVH) may occur in one third to one half of patients with spontaneous ICH as a result of arterial hypertension and/or small arteriolar degeneration. IVH is seen most often with thalamic, putaminal, or caudate nucleus hemorrhages, which can extend medially a short distance directly into the lateral or third ventricles. IVH in these patients clearly has been associated with larger ICH, midline shift, and increased morbidity and mortality. Hypertensive hemorrhages in the cerebellum (see Images 2-3) tend to occur adjacent to the dentate nucleus or in the deep white matter, depending on the perforating branches of the superior cerebellar or posterior inferior cerebellar arteries. Expansion of the hematoma may result in rupture into the fourth ventricle or extension into the contralateral side. Less frequently, hypertensive bleeds may occur in the cerebral white matter. Presentation Compared to the chronic effects of hypertension, relatively sudden elevations in blood pressure may cause neurologic consequences via a different mechanism. An acute episode of severe hypertension can cause breakdown of the blood-brain barrier, resulting in increased vascular permeability and focal edema. This may occur especially at blood pressure levels greater than 220/140, because the brain is no longer protected by autoregulation above this pressure. This possibly contributes to hypertensive encephalopathy. The more vulnerable areas are primarily the regions supplied by the posterior circulation where less sympathetic control of autoregulation exists. This situation may be aggravated by the thickened arteriolar walls of chronic hypertension, which do not allow normal vasoconstriction. In turn, this may cause cerebrovascular autoregulation to reset at higher pressures. Findings of capillary damage and vascular necrosis have been identified in situations of hypertensive encephalopathy and eclampsia. Thickened walls also increase vascular resistance. Consequently, collateral reserve is decreased, predisposing the brain to ischemic events.7,8 Potter et al evaluated the use of labetalol and lisinopril, compared with placebo, in patients with increased blood pressure (>160 mm Hg systolic) following stroke. There was no evidence of early neurologic deterioration in the patients receiving treatment, and there was a 50% decrease in 3-month mortality. The authors concluded that using labetalol and lisinopril to lower blood pressure after acute stroke can reduce mortality, as well as potential disability.9 Preferred Examination CT is efficient and sensitive in detecting ICH. This test may be followed by MRI to evaluate for possible underlying lesions and to gain more detailed information about a hemorrhage.10 Differential Diagnoses Other Problems to Be ConsideredUnderlying brain lesions (ie, tumor, vascular malformation)Ruptured aneurysm
Do you have any story's or suggestions that are relevant?Do you have a great story about this? Share it! Click here to leave brain hypertension and return to perfect brain homepage Keyword: Brain hypertension, brain hypertension, brain hypertension, Brain hypertension, Brain hypertension, Brain hypertension, Brain hypertension, Brain hypertension, Brain hypertension,
|